News & Announcements
Believe it: Hyperbaric therapy uses unique treatment to heal St. Luke’s patients

Cassidy Ihouma in the chamber with her daughter, Linnie.
By Chris LangrillLast Updated January 16, 2026
In a way, it looks so futuristic. And sometimes, the results make it feel otherworldly.
Hyperbaric oxygen therapy allows patients to breathe medical-grade oxygen while inside a pressurized chamber. The higher pressure forces more oxygen into the bloodstream, dissolves it into plasma and carries it to areas starved of oxygen.
It didn’t take long for St. Luke’s safety director Steve Richardson to become a believer after it became part of the care options at St. Luke’s more than 20 years ago.
“When we first started it was new for the hospital,” Richardson said. “We had only been open for about a year when we got an after-hours crush injury. He was an 18- to 19-year-old … and he was out working and a 2,000-pound battery fell on his foot. We put him in the chamber, and you knew exactly what was going to happen after the first treatment.
“You knew what was dark and dusky in his foot was going to have a hard time healing. What was bright and pink, you knew the blood flow was getting to it. It was amazing to me to watch. His toes went mummified, but the hyperbaric saved the upper part of his foot. So, he lost a few toes, but not the whole foot. Results like that are always the goal.”
Some of the more common conditions treated include diabetic food ulcers and nonhealing wounds, crush injuries, radiation tissue damage, carbon monoxide poisoning, decompression sickness (the bends) and chronic bone infections.
St. Luke’s Wound Care has clinics in Wood River, Twin Falls and McCall, with hyperbarics in Meridian and Boise. Check out our recent story on a Wood River patient who has benefited from the wound care team in her recovery after an accident.

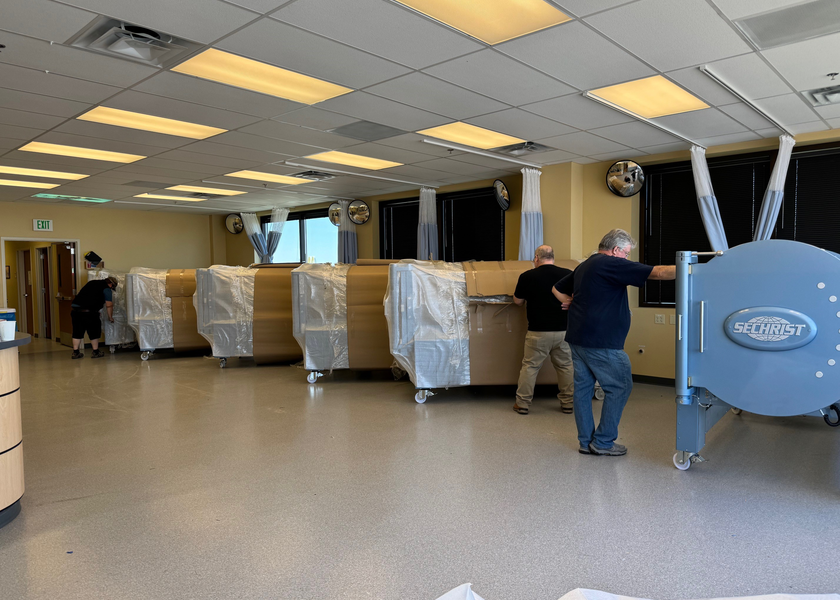
Shannon House with some of the Wound Care Team on new chamber delivery day.
“We treat only the approved indications by UHMS (Undersea & Hyperbaric Medical Society) and there are currently (15) approved indications,” said Shannon House, supervisor of St. Luke’s Wound and Hyperbarics, who will take the role of president of the Baromedical Nurses Association in May. “The ones we see the most are radiation injuries. That includes people who have had cancer treatments and have had radiation. … It can create a lot of problems with your body, because it doesn’t tolerate radiation.”
Over the years, House has seen the variety of ways hyperbaric therapy can be beneficial for St. Luke’s patients.
“With carbon monoxide, we’re saving patients from permanent neurological damage,” she said. “You can even see when someone comes in with carbon monoxide poisoning how much clearer they are by the end of their treatment that first day.
“I’ve seen very terrible foot wounds that I never would have thought would heal go on to heal. … In cases of prostate cancer, we’re the last option because if we can’t stop the bleeding they are going to lose the bladder.”
Despite being a part of the St. Luke’s Health System for more than two decades, the staff says there is sometimes an aura of mystery – and misunderstanding – surrounding hyperbarics. Richardson said he’s educated non-St. Luke’s physicians that it isn’t “voodoo.”
“We always joke that … people don’t know we exist,” House said.
House said she thinks it’s important that people know that hyperbaric therapy is a safe, viable option offered by St. Luke’s. Of note, patients are not left alone while in the chamber.
All St. Luke’s staff in the clinics are certified in hyperbarics as a specialty. Additionally, the clinic is accredited from the UHMS with distinction.
“We have a long process where we make sure that there is no reason that we couldn’t safely put someone in a chamber. Not everyone qualifies,” House said.
In June of 2024, St. Luke’s showed its commitment to hyperbaric therapy by acquiring six new chambers in Meridian. Crews had to use a crane to get the chambers into the clinic, which is on the fourth floor of the Portico building near St. Luke’s Meridian Medical Center.
“That’s well over $1 million,” Richardson said. “That’s quite the investment.”