Bronchoscopy
Test Overview
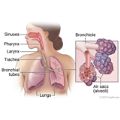
Bronchoscopy is a procedure that allows your doctor to look at your airway through a thin viewing device called a bronchoscope. During a bronchoscopy, your doctor will examine your throat, larynx, trachea, and lower airways.
This procedure may be done to diagnose problems with the airway, the lungs, or the lymph nodes in the chest. It may also be done to treat problems such as an object or growth in the airway.
There are two types of bronchoscopy.
- Flexible bronchoscopy.
-
It uses a long, thin, lighted tube to look at your airway. The flexible bronchoscope is used more often than the rigid bronchoscope. That's because it usually does not require general anesthesia, is more comfortable for the person, and offers a better view of the smaller airways. It also allows the doctor to remove small samples of tissue (biopsy).
- Rigid bronchoscopy.
-
It's usually done with general anesthesia and uses a straight, hollow metal tube. It is used:
- When there is bleeding in the airway that could block the flexible scope's view.
- To remove large tissue samples for biopsy.
- To clear the airway of objects (such as a piece of food) that can't be removed with a flexible bronchoscope.
Special procedures, such as widening (dilating) the airway or destroying a growth using a laser, are usually done with a rigid bronchoscope.
Why It Is Done
Bronchoscopy may be used to:
- Find the cause of airway problems, such as bleeding, trouble breathing, or a long-term (chronic) cough.
- Take tissue samples when other tests, such as a chest X-ray or CT scan, show problems with the lung or with lymph nodes in the chest.
- Diagnose lung diseases by collecting tissue or mucus (sputum) samples for examination.
- Diagnose and determine the extent of lung cancer.
- Remove objects blocking the airway.
- Check and treat growths in the airway.
- Control bleeding.
- Treat areas of the airway that have narrowed and are causing problems.
- Treat cancer of the airway using radioactive materials (brachytherapy).
How To Prepare
Procedures can be stressful. This information will help you understand what you can expect. And it will help you safely prepare for your procedure.
Preparing for the procedure
- Your doctor will tell you how soon before the procedure to stop eating and drinking. Follow the instructions exactly about when to stop eating and drinking, or your procedure may be canceled.
- Be sure you have someone to take you home. Anesthesia and pain medicine will make it unsafe for you to drive or get home on your own.
- Understand exactly what procedure is planned, along with the risks, benefits, and other options.
- Tell your doctor ALL the medicines, vitamins, supplements, and herbal remedies you take. Some may increase the risk of problems during your procedure. Your doctor will tell you if you should stop taking any of them before the procedure and how soon to do it.
- If you take a medicine that prevents blood clots, your doctor may tell you to stop taking it before your procedure. Or your doctor may tell you to keep taking it. (These medicines include aspirin and other blood thinners.) Make sure that you understand exactly what your doctor wants you to do.
- Make sure your doctor and the hospital have a copy of your advance directive. If you don't have one, you may want to prepare one. It lets others know your health care wishes. It's a good thing to have before any type of surgery or procedure.
How It Is Done
You may be asked to remove dentures, eyeglasses or contact lenses, hearing aids, wigs, makeup, and jewelry before the bronchoscopy procedure. You will empty your bladder before the procedure. You will need to take off all or most of your clothes (you may be allowed to keep on your underwear if it does not interfere with the procedure). You will be given a cloth or paper covering to use during the procedure.
The procedure is done by a thoracic surgeon or a pulmonologist and an assistant. Your heart rate, blood pressure, and oxygen level will be checked during the procedure.
A chest X-ray may be done before and after the bronchoscopy.
Flexible bronchoscopy
During this procedure, you will lie on your back on a table with your shoulders and neck supported by a pillow, or you will recline in a chair that resembles a dentist's chair. Sometimes the procedure is done while you are sitting upright.
You will be given a sedative to help you relax. You may have an intravenous line (IV) placed in a vein. You will remain awake but sleepy during the procedure.
Before the procedure, your doctor usually sprays a local anesthetic into your nose and mouth. This numbs your throat and reduces your gag reflex during the procedure. If the bronchoscope is to be inserted through your nose, your doctor may also place an anesthetic ointment in your nose to numb your nasal passages.
Your doctor gently and slowly inserts the thin bronchoscope through your mouth (or nose) and advances it to the vocal cords. Then more anesthetic is sprayed through the bronchoscope to numb the vocal cords. You may be asked to take a deep breath so the scope can pass your vocal cords. It is important to avoid trying to talk while the bronchoscope is in your airway.
An X-ray machine (fluoroscope) may be placed above you to provide a picture that helps your doctor see any devices, such as forceps to collect a biopsy sample, that are being moved into your lung. The bronchoscope is then moved down your larger breathing tubes (bronchi) to examine the lower airways.
If your doctor collects sputum or tissue samples for biopsy, a tiny biopsy tool or brush will be used through the scope. A salt (saline) fluid may be used to wash your airway, then the samples are collected and sent to the lab to be studied.
Finally, small biopsy forceps may be used to remove a sample of lung tissue. This is called a transbronchial biopsy.
Rigid bronchoscopy
This procedure is usually performed under general anesthesia. You will lie on your back on a table with your shoulders and neck supported by a pillow.
You will be given a sedative to help you relax. You will have an intravenous line (I.V.) placed in a vein. Once you are asleep, your head will be carefully positioned with your neck extended. A tube (endotracheal) will be placed in your windpipe (trachea) and a machine will help you breathe. Your doctor then slowly and gently inserts the bronchoscope through your mouth and into your windpipe.
If your doctor collects sputum or tissue samples for biopsy, a tiny biopsy tool or a brush will be inserted through the scope. A salt (saline) fluid may be used to wash your airway, then the samples are collected and sent to the lab for biopsy.
Recovery after bronchoscopy
Bronchoscopy by either procedure usually takes about 30 to 60 minutes. You will be in recovery for 1 to 3 hours after the procedure. Following the procedure:
- Do not eat or drink anything for 1 to 2 hours, until you are able to swallow without choking. After that, you may resume your normal diet, starting with sips of water.
- Spit out your saliva until you are able to swallow without choking.
- Ask your doctor when you can drive again.
- Do not smoke for at least 24 hours.
How long the test takes
A bronchoscopy (either flexible or rigid) usually takes about 30 to 60 minutes. You will be in recovery for 1 to 3 hours after the procedure.
How It Feels
If you have general anesthesia, you will feel nothing during the procedure. Oxygen is usually given through a small tube placed in your nose if you are awake during the procedure.
You may be able to feel pressure in your airway as the bronchoscope is moved from place to place. You may gag or cough. Your airway will not be blocked. But if you feel discomfort, let your doctor know.
Risks
Bronchoscopy is generally a safe procedure. Complications are rare. But your doctor will discuss any risks with you. Complications that may occur include:
- Spasms of the bronchial tubes, which can impair breathing.
- Irregular heart rhythms (arrhythmias).
- Infections, such as pneumonia. These can usually can be treated with antibiotics.
- Ongoing hoarseness.
If a biopsy was done during bronchoscopy, complications that may occur include:
- A tear in the lung from the biopsy forceps used to collect a tissue sample. This will allow air to flow into the pleural space and cause a partial collapse of the lung (pneumothorax).
- Bleeding caused by the biopsy forceps used to collect the tissue.
- An infection from the biopsy procedure.
- A very small chance of death.
Results
Your doctor may discuss your results with you soon after the procedure. Test results on any biopsy samples are usually available in 2 to 4 days.
|
Normal: |
The large airway leading to the lungs and the breathing tubes in the lungs appear normal. There are no objects, thick secretions, or growths. |
|---|---|
|
Abnormal: |
An object, thick secretions, or growths are blocking your airway. |
|
Tissue sample shows a lung infection or disease, such as tuberculosis or lung cancer. |
Related Information
Credits
Current as of: July 31, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: July 31, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.