Abnormal Uterine Bleeding
Condition Basics
What is abnormal uterine bleeding?
Abnormal uterine bleeding is irregular bleeding from the uterus. It may be bleeding that is heavier, lighter, or lasts longer than your usual period. Or it may be bleeding that doesn't occur at your regular time. Let your doctor know if your bleeding is different than usual. They can check for problems.
What causes it?
Abnormal uterine bleeding has many causes. It's sometimes caused by changes in hormone levels. It can also be caused by problems such as growths in the uterus or clotting problems. In rare cases, it may be caused by a more serious problem, such as cancer. Sometimes the cause of the bleeding isn't known.
What are the symptoms?
Symptoms of abnormal uterine bleeding include periods that happen more or less often, seem lighter or heavier than normal, or last longer. Symptoms can also include bleeding when you don't expect to, such as between periods or after sex.
How is it diagnosed?
Your doctor will ask how often, how long, and how much you have been bleeding. You may also have a pelvic exam, a urine test, blood tests, and possibly an ultrasound. Your doctor may also take a tiny sample (biopsy) of tissue from your uterus for testing.
How is abnormal uterine bleeding treated?
There are many ways to help treat abnormal uterine bleeding. Some are meant to return the menstrual cycle to normal. Others are used to reduce bleeding or to stop monthly periods. Treatments can include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil, Motrin).
- Hormone therapy. This can include hormonal birth control or other medicines.
- Hysteroscopy. This procedure can remove polyps or fibroids.
- Surgery, such as endometrial ablation or hysterectomy. It may be done when other treatments don't work.
Sometimes symptoms get better without treatment. After a doctor rules out serious problems, some people choose to wait and see if symptoms get better on their own.
Health Tools
Health Tools help you make wise health decisions or take action to improve your health.
What Increases Your Risk
Risk factors (things that increase your risk) for abnormal uterine bleeding include:
- Age. Abnormal uterine bleeding is more common during the teen years and around menopause.
- Weight. Being overweight or underweight can increase your risk for abnormal uterine bleeding.
- Genetics. Having a family history of abnormal uterine bleeding may increase your risk.
Some people have abnormal uterine bleeding even though they have no risk factors.
Prevention
Abnormal uterine bleeding usually can't be prevented. But being under or over your recommended weight can affect your hormone production. This can increase your risk for irregular menstrual bleeding. In some cases, staying at a healthy weight may help prevent abnormal uterine bleeding.
Explore more
Watch
Symptoms
Symptoms of abnormal uterine bleeding include:
- Getting your period more or less often than normal. A normal adult menstrual cycle is about 21 to 35 days long. A normal teen cycle is about 21 to 45 days.
- Periods that last longer than 7 days.
- Bleeding during your period that is lighter or heavier than usual. With heavy bleeding, you may soak through your pads or tampons often.
- Bleeding when you don't expect to, such as between periods or after sex.
What Happens
Abnormal uterine bleeding may occur from the teen years until after age 40. In teens, it may improve as menstrual cycles get more regular. Depending on the cause, it may resolve with treatment or on its own.
When to Call
Any change in your menstrual pattern or amount of bleeding that affects your daily life should be checked by a doctor. This could include:
- Getting your period more or less often than normal. A normal adult menstrual cycle is about 21 to 35 days long. A normal teen cycle is about 21 to 45 days.
- Periods that last longer than 7 days.
- Periods that are lighter or heavier that usual. With heavy bleeding, you may soak through your pads or tampons often.
- Not getting your period for more than 3 months.
- Bleeding when you don't expect to, such as between periods or after sex.
Check your symptoms
Exams and Tests
Your doctor will review your history of symptoms and menstrual periods. Your doctor will ask how often, how long, and how much you have been bleeding. (If you can, bring with you a record of the days you were bleeding, how heavy or light the flow was, and how you felt each day.)
You may also have tests to help find the cause of your symptoms and to rule out serious health problems. These tests may include:
- A pelvic exam.
- A fluid sample from your cervix or vagina.
- A Pap or HPV test.
- A urine test.
- A blood test.
- An ultrasound.
- A biopsy. For this test, your doctor takes a tiny sample of tissue from your uterus.
Learn more
Treatment Overview
Abnormal uterine bleeding usually can be treated with medicine, hormone therapy, or both. Surgery may be done for bleeding that can't be controlled with medicine or hormones.
Acute, severe uterine bleeding
Severe uterine bleeding is often treated as an emergency. It may be treated with medicine, such as high-dose estrogen. Or it may be treated with a procedure, such as a dilation and curettage (D&C). When needed, a blood transfusion may be used to quickly restore blood volume.
Later, you and your doctor can choose a treatment that is safe for the longer term.
Ongoing uterine bleeding
Your treatment choices depend on your age, the cause of your bleeding, and if you plan to get pregnant in the future. Treatments include:
- Hormone therapy
-
- Birth control pills, patch, or ring. These can help control your cycle and reduce menstrual bleeding and cramping.
- Hormonal IUD. This is a birth control device that your doctor places inside your uterus. It releases progestin and can reduce bleeding and cramping.
- Progestin-only birth control, such as mini-pills, implants, or shots. These types of birth control can reduce bleeding and cramping.
- Progestin pills. These are progestin-only pills that can help reduce bleeding but don't prevent pregnancy.
- Non-hormonal medicines
-
- Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil, Motrin). Taking an NSAID can reduce bleeding and pain during your period.
- Tranexamic acid (such as Lysteda). This is a medicine that reduces bleeding by helping your blood to clot.
- Surgery
-
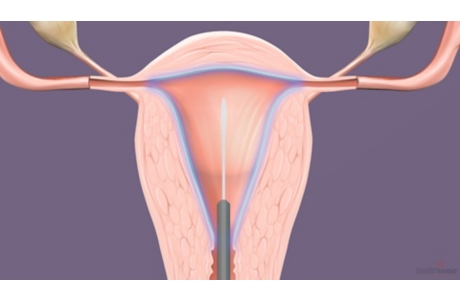
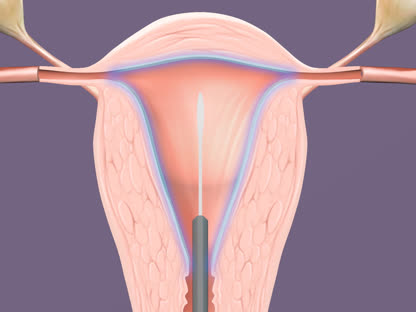
- Hysteroscopy. This procedure is done to diagnose abnormal uterine bleeding. But it can also treat some problems at the same time. For example, fibroids or polyps may be removed during this procedure.
- Endometrial ablation. This procedure destroys the endometrium. This reduces or stops uterine bleeding. But it isn't an option if you would like to get pregnant in the future.
- Hysterectomy, a surgery to remove the uterus. This may be an option if heavy bleeding can't be controlled or when the cause of bleeding can't be found and treated. You won't be able to get pregnant after a hysterectomy.
Sometimes symptoms get better without treatment. After a doctor rules out serious problems, some people choose to wait and see if symptoms get better on their own.
Learn more
Watch
Self-Care
You can use home treatment for some problems related to abnormal uterine bleeding.
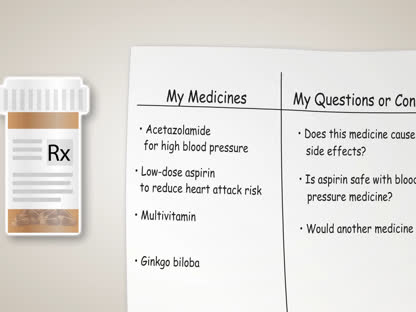
A nonsteroidal anti-inflammatory drug (NSAID), such as over-the-counter ibuprofen (Advil, Motrin), can help reduce bleeding and menstrual pain. It works best when you start taking it 1 to 2 days before you expect bleeding or pain to start. If you don't know when your period will start next, take your first dose of an NSAID as soon as bleeding or premenstrual pain starts. Be safe with medicines, and follow your doctor's instructions.
Irregular menstrual bleeding can lead to low levels of iron in the blood. This condition is known as iron deficiency anemia. You can help prevent anemia by increasing the amount of iron in your diet.
Explore more
Medicines
Medicines can help stop or reduce bleeding. They can also help make your bleeding more regular.
Medicine choices
Several hormone treatments can manage bleeding.
- Birth control pills, patch, or ring.
-
These can help control your cycle and reduce bleeding and cramping.
- The levonorgestrel intrauterine device (IUD).
-
This is a birth control device that your doctor places inside your uterus. It releases progestin and can reduce bleeding and cramping.
- Progestin-only birth control.
- This can include mini-pills, implants, or shots. These types of birth control can reduce bleeding and cramping.
- Progestin pills (synthetic progesterone.).
-
These are progestin-only pills that can help reduce bleeding but don't prevent pregnancy.
- Estrogen.
-
In some severe or urgent cases, estrogen may be used to reduce bleeding.
Other non-hormonal medicines can also be used for treatment.
- Nonsteroidal anti-inflammatory drugs (NSAIDs).
- Taking an NSAID can reduce bleeding and pain during your period.
- Tranexamic acid.
- This is medicine reduces bleeding by helping your blood to clot.
Learn more
Watch
Surgery
Surgery may be done to treat bleeding that isn't controlled with medicine.
Surgery choices
Several procedures are used to treat bleeding.
- Hysteroscopy can be used to diagnose and treat bleeding at the same time. A lighted viewing scope is placed through the vagina and cervix and into the uterus. Biopsies can be taken where there is bleeding. The bleeding can be treated with either a laser beam or electric current.
- Hysterectomy is the removal of the uterus. It may be done when a biopsy shows abnormal cell changes or cancer. It also can be done when bleeding can't be controlled or when the cause of long-term bleeding can't be found and treated.
- Endometrial ablation is another choice when other medical treatments don't work or when you or your doctor have reasons for not using other treatments. It scars the uterine lining, so it is not an option if you are planning to become pregnant.
Learn more
Watch
Related Information
Credits
Current as of: April 30, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: April 30, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.