“Especially For You”: New Menu for Boise Mother-Baby Unit
Staff from the Boise mother-baby unit noted a trend in patient reviews related to available meal options. Patients were requesting items with a higher protein content and larger portions to meet their increased caloric needs. They asked for a wider selection of beverages, fresh salads and comfort foods, too. These findings were reinforced when the Press Ganey scores were reviewed by the Women’s Services nursing leadership team.
An interdisciplinary work group was established, and St. Luke’s food and nutrition service operations team, chefs, dietitians, the call center, nursing leadership and bedside nursing staff provided input. This collaboration led to the creation of a new menu supplement and the design of a coffee bar area for patients and their personal support teams.
Choices on the new menu range from healthy garden selections to satisfying comfort food. The presentation is restaurant style with portions large enough to fill up even the hungriest maternity patient. Late-night options were expanded, and a variety of protein-packed snacks were made available for immediate or scheduled in-room delivery. The coffee bar includes a variety of coffee pods, gourmet tea, flavored creamers and syrups to allow for drink customization.

This menu, launched mid-November 2023, was named “Especially for You,” so patients know their experience is our priority. Although this project is new, patient experience scores have already started to rise, and patients are voicing appreciation for the expanded menu and coffee station.
When well-established, the goal is to spread this initiative throughout the health system to reach all maternity patients. Collaboration on this initiative demonstrates how St. Luke’s is unified in our pursuit of excellence. From the kitchen to the bedside, we work as a team to provide patient-centered care.
New Class Makes a Difference for Patients With Acute Kidney Disease
St. Luke’s did not have a defined process for patient education in terms of dialysis options or kidney transplant. Patients were being diagnosed with advanced kidney disease and would only get a very brief introduction to dialysis and the process for it, then be asked to make a quick decision on a treatment plan.
Maria Gumucio-Powell, BSN, RN, kidney care coordinator for St. Luke’s Clinic – Kidney and Hypertension in Boise, Meridian and Nampa, was tasked with finding a solution that would provide patients a more expansive overview of each dialysis type, communicated in a setting with opportunity for bidirectional feedback, which would support better decision-making regarding care.
Maria created the Options Class, which she teaches for all patients who are near or ready to start dialysis. The class is delivered one-on-one with the patient (and a family member/support person, if needed), so each class can be tailored to the patient’s situation and allow for dialogue regarding questions, concerns and fears.
There has been a steady increase of patients attending the Options Class since its launch, and, in 2023, approximately 140 patients attended. In addition to increasing participation, there has been an increased number of kidney transplant referrals and patients who are active on the kidney transplant list.
Hospice Nurse Advocates for Innovative Comfort Management
Hospice nurse Asia Christensen, BSN, RN, had a patient on her caseload who was receiving lymphedema therapy, related to the patient’s metastatic cancer diagnosis, in the outpatient wound clinic. The patient was becoming too weak to leave home but had achieved great comfort with the therapy and didn’t want to discontinue it.
The lymphedema therapy could be provided in the home setting with a prescribed pump system, so the wound clinic placed a referral to a local durable medical equipment (DME) company for a lymphedema management system. However, insurance denied coverage.
Asia went to work. She was able to present the patient’s need to the hospice collaborative, where it was decided that hospice should cover this item, though previously it was not an item on the DME hospice formulary.
Unfortunately, the patient passed away before being able to have the
system in her home, but Asia’s advocacy for her patient will allow future
patients to have access to a previously non-covered item.

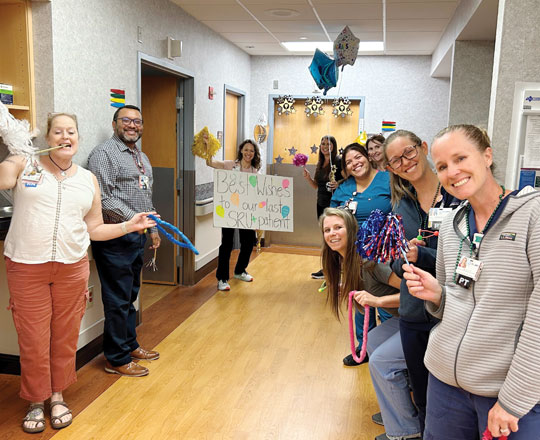
Jerome Embraces Swing Bed Status by Celebrating Discharge With a Graduation Ceremony
St. Luke’s Jerome admits patients predominately in swing beds, which is a service that allows patients to transition from acute care to skilled nursing care without leaving the hospital. On average, they are admitted for 14 days for skilled therapy needs.
Stacey Squires, MS, RN, recognized how rewarding it is to see a patient’s progress through the swing bed program. She proposed the team celebrate each patient’s hard work with a graduation ceremony upon discharge.
The Jerome team got together and gathered supplies. In November 2023, Jerome held its first discharge graduation ceremony. The patient was admitted for physical and occupational therapy. He struggled when he first arrived. He was very stiff from limited mobility due to pain—and was in excruciating pain with any movement.

Over the course of a few weeks, his healing progressed. The patient was soon able to walk with little pain, and the team got to see his sweet, gentle personality emerge. On his day of graduation, nursing, environmental services, social work and therapy staff lined the hallway clapping as he left the unit.
He wore a celebratory hat, staff had party blowers, and the graduation song was playing. He smiled and shook the staff members’ hands as he left the building. When he got outside, he started crying and stated he had never felt that loved. He was so appreciative of the care he received at St. Luke’s and thankful that staff took the time to celebrate his success.
The team continues to celebrate each swing bed patient’s discharge with a graduation ceremony that acknowledges the patient’s successful transition back to home.

Wood River Operating Rooms Are Designated Smoke Free
The Association of Perioperative Registered Nurses (AORN) is the industry leader in evidence-based best practice guidelines that support safe surgery for both patients and staff. Near the end of 2022, the St. Luke’s Wood River surgical team learned about AORN’s national “Go Clear” campaign, aimed at reducing and eliminating surgical smoke in the operating rooms.
During surgery, the use of cautery produces a smoke plume that, when inhaled, can lead to caustic health impacts ranging from mild respiratory issues to cancer. While those closer to the surgical field (surgeons and technicians) are at greater risk, all individuals—including the patient—are at risk for smoke inhalation.
To mitigate this risk, the Go Clear campaign challenges hospitals to implement a smoke-free environment through use of disposable smokeevacuation instruments in conjunction with specialized smoke-filtration devices. St. Luke’s Wood River chose to accept the challenge and pursue the Go Clear Award™ by designing smoke-free operating rooms.
After testing several devices, bringing in appropriate supplies, and educating both staff and providers, the Wood River OR team established a new workflow that reduces the frequency of smoke plumes during surgery. Over a 12-week audit period, the team submitted data demonstrating compliance at St. Luke’s Wood River.
At the 2023 AORN Conference, St. Luke’s Wood River was recognized with the AORN Go Clear Award. Based on compliance data, they even achieved the Gold Level (highest) recognition. St. Luke’s Wood River became not only the first in the system but the first hospital in Idaho to win this award.
Wood River Emergency Department Improves Time From Order to Antibiotic Treatment for Sepsis
In 2023, St. Luke’s Wood River Emergency Department rolled out an important quality project focused on sepsis recognition and treatment.
Inspired by Kristina Martinez, MSN, RN, sepsis program manager, and with guidance from Alecia Gorringe, BSN, MHI, RN, CPHQ, quality manager, the ED committed to complete all sepsis huddles and improve their order-to-antibiotics time. The team was already doing well on their huddles but had room to improve on time from order to antibiotics administration.
The system goal is 30 minutes—the Wood River ED team set a goal of 10 minutes or less! Recognizing that this project would not be successful without full collaboration between the nurses and doctors, leaders worked on robust education for the whole team.
Leaders also included a healthy side of competition. Each month, the team celebrated their “Sepsis Superheroes” and announced their exceptional times in the Recognition Hallway. From August to December 2023, the median order-to-antibiotics time ranged from 13 to 17 minutes. The standout times were extraordinary. On three occasions, the order to antibiotics was only one minute.
This could not have been accomplished without real-time collaboration and communication between the ED providers and the nurses. We are very proud of our Wood River ED Sepsis Superheroes!


Improved Whiteboards Help Patients Understand Fall Risk
St. Luke’s Meridian medical-surgical unit partnered with the system Fall Prevention Collaborative to pilot new whiteboards aimed at decreasing the number of falls with injury, which are the leading serious safety event at St. Luke’s.
The whiteboards allow clinical staff to communicate with fall-risk patients through an educational, nurse-driven design. Clinical staff worked closely with the performance improvement team to design and create the boards based on current workflows.
The new boards communicate individualized patient mobility levels, risk factors, a fall safety plan and movement goals. Clinical staff organized the elements of the board in the way that works best for them and the patients. The whiteboards are in English on one side and Spanish on the other. They will be placed in a prominent position within a patient’s room so the care team, patient, and the patient’s family can easily access and discuss the information.
The new signs encourage patients to be proactive and help them understand the fall risks that might be associated with their hospitalization, even if they historically haven’t thought of themselves as at risk of falling. This innovative strategy increases patient awareness of fall-risk interventions and has resulted in reduced patient falls.
The St. Luke’s Magic Valley Inpatient Rehabilitation Unit Earns #1 Rank in Idaho
U.S. News and World Report recently ranked the inpatient rehabilitation unit (IRU) at St. Luke’s Magic Valley, Gwen Neilsen Anderson Rehabilitation Center, as first in Idaho. They consider categories such as discharges of patients to home, prevention of hospital readmission during and after rehabilitation stays, rate of flu vaccines, CARF accreditation and patient services in their ranking decision.
Nursing played a big role on the road to achieving this top rating. Inpatient rehabilitation nursing is unique from other nursing disciplines: nurses oversee the patients’ medical needs, learn and respond to cues, and encourage the patients to achieve milestones and goals on their own. Nurses also teach patients new skills and, often, reteach skills patients once had but are now unable to accomplish due to their conditions.
The IRU uses a strong interdisciplinary team approach. Nurses, doctors and therapists work hand in hand helping patients learn to navigate life in new ways and achieve independence.
St. Luke’s is proud of the Magic Valley IRU staff for earning the number one
rating. It highlights the work they accomplish to improve the lives of the
people in the community.

Team Nursing: New Care Delivery Model Supports Patient-Centered Care
St. Luke’s most widely used care model has been a version of primary care nursing with registered nurses assigned to patients, assisted by certified nurse assistants, and a focus on continuity of RN assignments and maintenance of ratios from shift to shift. While this model has worked well in the past, the future workforce is uncertain, so there was a need to find a more flexible and sustainable model moving forward.
To meet these challenges head on, St. Luke’s Nursing and Patient Care Center of Excellence constructed an evidence-based team nursing (TN) model designed to adapt to unit size and caregivers at all levels of education and experience. TN shifts the care delivery to a shared responsibility within defined roles, creating a nursing model that provides flexibility for use in a variety of settings and fosters an environment that elevates the care experience for both patients and staff.
The TN model establishes a sustainable framework that nurtures new RNs through mentorship, teamwork and skill development with the adaptability to be implemented in a variety of nursing units. There is also an opportunity to customize depending on staff available.

Nampa Telemetry Pilots Team Nursing Model in January 2023
The Nampa telemetry unit took the lead in piloting the first implementation of a TN model, aimed at rebuilding the workforce by supporting new graduate RNs and improving the overall practice environment. The TN model focused on intentional mentorship, leveraging the expertise of experienced RNs, and shifted staffing assignments to shared responsibility based on skills and patient needs, allowing for increased flexibility.
Throughout the process, Nampa proactively managed change, conducted training sessions and gathered continuous feedback to ensure success.
Leaders measured staff commitment and unit function improvements to evaluate the impact of the model. Nampa telemetry showed positive results, including increased staff collaboration and reduced new RN orientation hours. There was also a significant improvement in pulse poll results when looking at staff’s responses to the “intend to work at St. Luke’s 2-3 years from now” and “feeling like I belong” survey questions.
The valuable insights and best practices from the initial implementation
were shared throughout the organization, contributing to knowledge
dissemination and organizational learning.

Meridian Telemetry Implements New Model in February 2023
The Meridian telemetry unit was the second unit to go live with the new TN model. Since initiating TN, Meridian telemetry has significantly decreased reliance on contract labor through retention as well as hiring both experienced and new nurses into core positions.
Meridian also introduced the role of LPNs into the TN model by working with local programs, which increased opportunities for LPN students in the hospital setting. Their knowledge and skills add value and have helped improve patient safety. Teamwork and collaboration also continue to improve with the integration of LPNs into the TN model.
Following the implementation of TN, Meridian telemetry data showed improvements in patient experience scores, a decrease in falls with injury, and—anecdotally based on nurse leader rounding—more confidence from new graduate nursing staff. Lessons learned from TN have added to the sustainable framework for other nursing units throughout the organization.

Magic Valley Inpatient Medical Unit Builds on Lessons and Implements Model in March 2023
In March 2023, the Magic Valley inpatient medical unit began work on a TN model utilizing LPNs. The challenging part of implementing the model was how to incorporate LPNs into the current team.
Buy-in from staff was essential. Finding a way to ensure the team remained inclusive of all was a key goal. To do this, leaders held several listening sessions, which allowed the team to ask questions and be a part of the process flows. The leadership team worked hard on learning the scope of practice for the LPNs and what St. Luke’s current policies and procedures allow.
This understanding guided development of the tools needed for an LPN to provide the best care for patients. The charge and team lead nurses developed an “assignment tool” to ensure the team, including LPNs and RNs, would receive balanced assignments based on both acuity and demands of the patients.
With the help of Clinical Learning and Student Services, the new employee clinical orientation (also known as NECO) was adapted, with elements included to ensure LPNs would develop skills needed to be successful at the bedside. Precepting of the LPNs was tailored to meet their individual needs as some were new graduates and some came from clinics, with varying amounts of experience.
The diligence involved in this work led to a successful implementation of
the TN model using the LPN and has expanded to the cardiopulmonary
unit in Magic Valley.
Download Full Copies of Our Nursing Annual Reports